By NEHA P. JAMES, DO
Vulvodynia describes a condition of chronic pain, irritation, or discomfort in the area around the vaginal opening. Symptoms are termed chronic when they persist for over three to six months. Vulvodynia most commonly affects women aged 18-25, but it can also be seen in older women and postmenopausal women. As many as one in six women in the U.S. will experience vulvodynia symptoms at some point in their lives.
What does vulvodynia feel like?
Patients who suffer from vulvodynia symptoms often report pain in the vulva that feels like burning, stinging, stabbing, or intense itching. They may also describe a sensation of rawness and extreme hypersensitivity in the skin. These symptoms can involve part or all the vulva, including but not limited to the vaginal entrance, the inner labia, the urethra, and the clitoris. The area may also look red and irritated in the mirror.
Some women find that symptoms flare with touch, making sexual penetration intolerable, while others find symptoms are triggered by activities like prolonged sitting or even by wearing underwear. This can make it difficult to sustain romantic relationships or be productive at work. Many women also report that symptoms worsen in times of high stress, creating a difficult cycle of stress and pain that greatly decreases quality of life.
What causes vulvodynia?
Vulvodynia can be caused by several different contributing factors. It’s important to work with an experienced pelvic pain physician to identify the causes that may apply to you. These include, but are not limited to:
- Vaginal infections or trauma
- Hormonal changes or imbalances
- Injury or irritation of the pelvic floor nerves
- Dysfunction of the pelvic floor muscles
How is vulvodynia diagnosed?
Your pelvic pain physician will perform a thorough evaluation to correctly identify vulvodynia and rule out other contributing conditions. This will include taking a detailed history of your symptoms, reviewing your medical conditions, past surgeries, and medications, discussing contributing factors such as trauma or infection, and doing a physical exam.
The physical exam for vulvodynia involves looking at the affected skin, assessing the surrounding pelvic floor nerves that give sensation to the area, and (if tolerable) gently applying pressure to the skin to check which areas are involved. The main goal of the exam is to collect information without triggering pain, so gentleness and communication are key.
How is vulvodynia treated?
Since vulvodynia can have many different contributing factors, it’s important to treat this condition using a holistic, multi-modal approach to see lasting improvement and resolution. Your pelvic pain physician can make recommendations about which medications and physical therapy treatments are the best fit for you. Your pelvic pain physician can also perform injections to the pelvic floor using ultrasound guidance to release tension in your muscles, decrease nerve-related inflammation, and improve blood flow to promote healing.
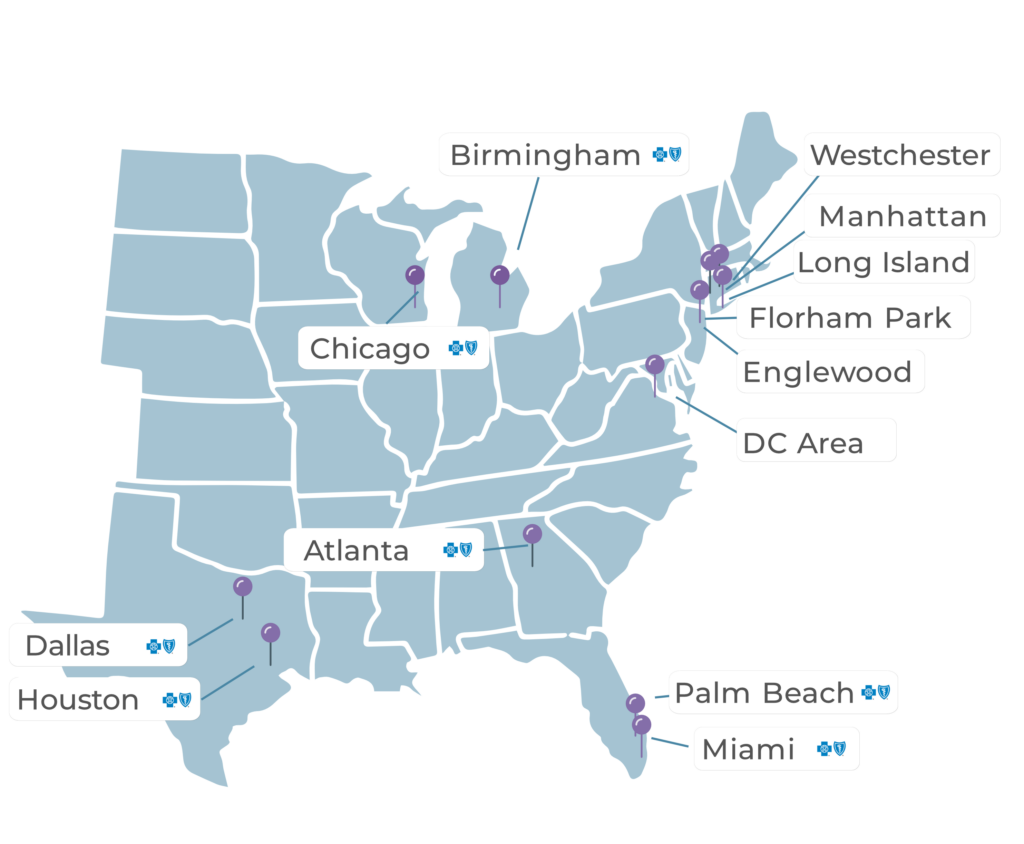
At PRM, our team takes a multi-modal approach to treating pelvic pain conditions such as vulvodynia. Our unique in-office, nonoperative, minimally invasive ultrasound guided approach to the pelvis is the first of its kind in the country. Our pelvic pain specialists can provide an internal evaluation and use ultrasound to guide treatment externally – bringing relief to pelvic pain sufferers everywhere. This is an office-based treatment with no anesthesia and no down time. Patients go on with their day directly after.

Would You Like to See a Specialist?
Call us at (646) 481-4998 or click to request a regular appointment.