By Allyson Augusta Shrikhande, MD, CMO
What is endometriosis?
Endometriosis is a chronic, hormone-dependent, systemic inflammatory disease characterized by the presence of endometrial like tissue outside of the uterine cavity. It is typically associated with pelvic pain and infertility.
How is endometriosis diagnosed?
We know that patients with endometriosis often suffer for many years and see multiple physicians and medical providers before receiving a diagnosis. In patients aged 18- 45, the average delay in diagnosis is 6.7 years. This may be secondary to the fact that endometriosis is a diagnosis of exclusion.
The gold standard for the diagnosis of endometriosis has been visual inspection by laparoscopy, preferably with histological confirmation. Because there is lack of a noninvasive test for endometriosis, there is often a significant delay in diagnosis of this disease.
What are the gastrointestinal symptoms that may occur with endometriosis?
The most common location for extragenital endometriosis is the bowel. Common gastrointestinal symptoms for endometriosis patients are:
- abdominal pain
- rectal pain
- bloating
- constipation
- difficulty evacuating stool
- straining with bowel movement
- splinting the posterior vagina
- anal digitation
- incomplete evacuation
- sense of anal blockage during defecation
- Dyschezia
- bowel frequency
In addition, some endometriosis patients complain about blood in their stool around their menstrual cycle.

Are you experiencing the symptoms of endometriosis?
Take PRM’s Endometriosis Symptoms Quiz to learn more
about your symptoms and what we can do to help.
How is endometriosis treated?
Currently there is no definitive cure for endometriosis however, therapy has three main objectives:
(1) to reduce pain
(2) to increase the possibility of pregnancy
(3) to delay recurrence for as long as possible

What are the treatment options for endometriosis?
Hormonal Treatment Options
One example of a hormonal treatment option is Elagolix (Orilissa). Elagolix is an oral, nonpeptide, gonadotropin-releasing hormone (GnRH) antagonist used to treat moderate to severe pain related to endometriosis. Inhibition of GnRH leads to estrogen suppression and subsequent dose-dependent inhibition of endometriotic proliferation.
Surgical Treatment Options
Surgical resection can be accomplished through therapeutic laparoscopic techniques using scissors, electrosurgical instruments, lasers, suture, and staplers.
Non-Surgical/Non-Hormonal Options
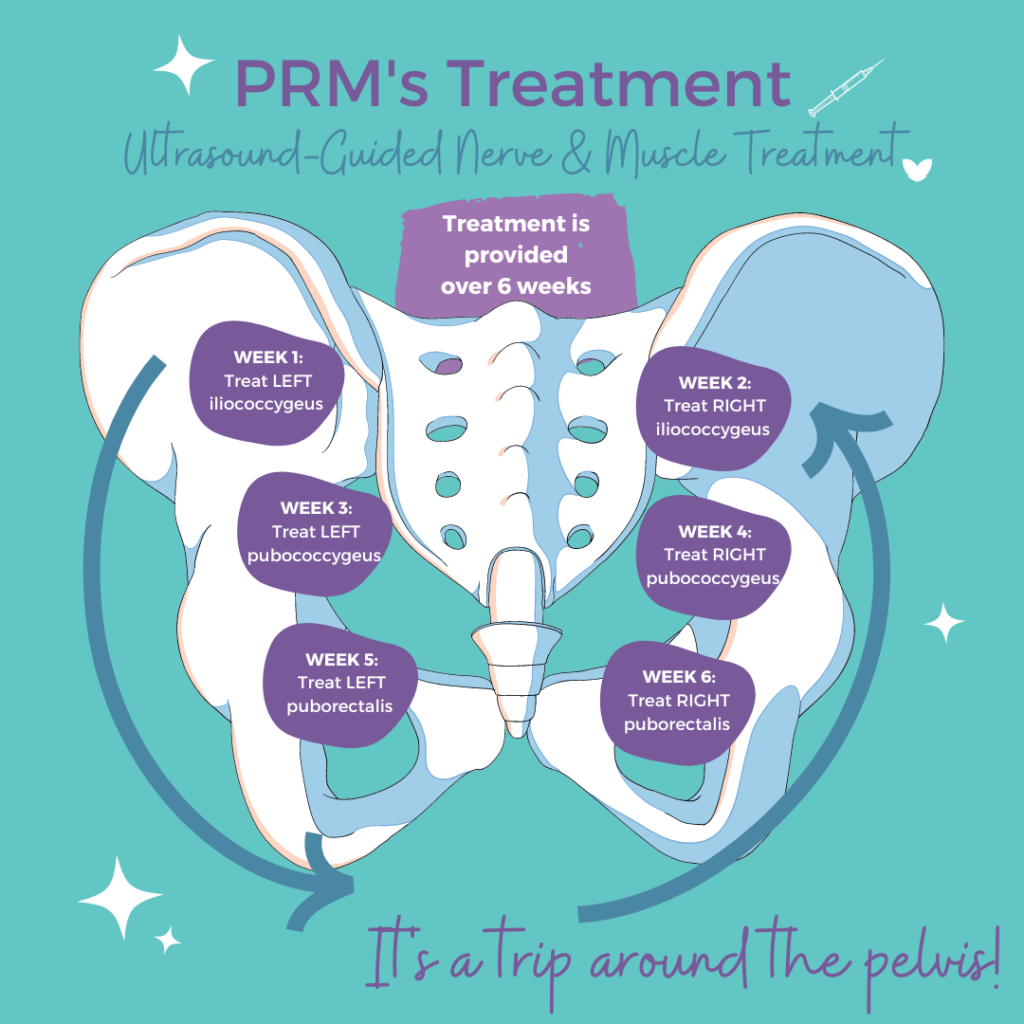
At PRM, we propose a non-operative neuromusculoskeletal approach in addition to the hormonal and surgical combination, to help reduce pelvic pain symptoms associated with endometriosis.
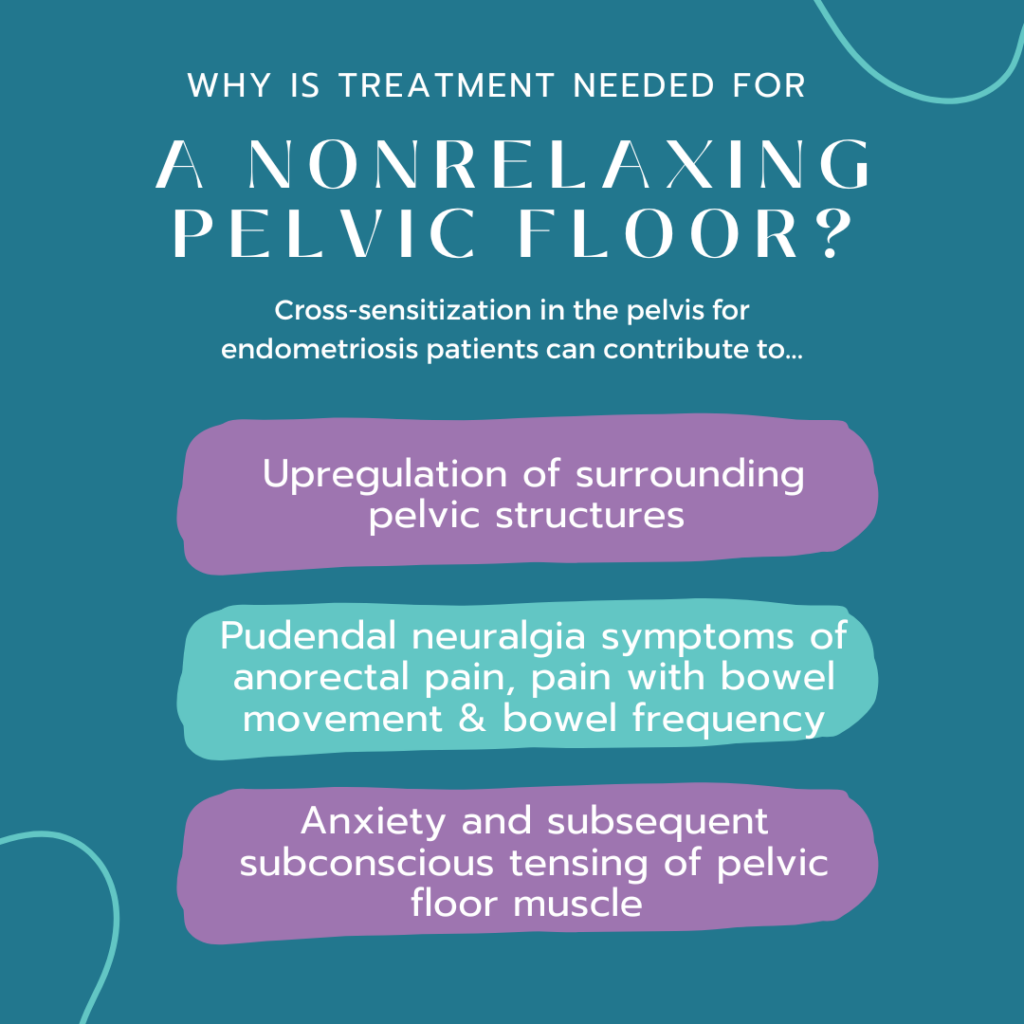
How Does Endometriosis Affect the Pelvic Floor?
Endometriosis can cause gastrointestinal symptoms via several mechanisms:
- Direct innervation of pelvic nerves
- Direct innervation of the bowel itself
- Stimulating a hypertonic pelvic floor
- Cross-sensitization, peripheral
- Central sensitization
Endometriosis can directly innervate pelvic nerves, particularly the pudendal nerve. This contributes to pudendal neuralgia symptoms of anorectal pain and pain with bowel movements. Innervation of the pudendal nerve also contributes to increased bowel frequency.
How Does Endometriosis Affect the bowel?
Endometriosis can also directly invade the bowel itself, contributing to bowel symptoms of constipation and pain with bowel movement. The presence of endometriosis in the pelvis can cause a secondary chronic guarding of pelvic floor musculature.
This chronic guarding state leads to nonrelaxing pelvic floor dysfunction and myofascial trigger points (MTrPs). A nonrelaxing pelvic floor, will cause symptoms:
- difficulty evacuating stool
- straining with bowel movements
- a sense of incomplete evacuation
- bloating
- constipation
The pelvic floor muscles in nonrelaxing pelvic floor dysfunction are short, spastic, weaker, and poorly coordinated. This leads to dyssynergic defecation, which occurs when the nerves and muscles within the pelvic floor do not function well enough to properly have a bowel movement.
PRM’s Approach to Treating Endometriosis and Gastrointestinal Issues
Our protocol aims to simultaneously reverse the pelvic floor myofascial pain and dysfunction, peripheral sensitization, and central sensitization that exists in endometriosis patients.
Our approach works in three ways:
- Reduce spontaneous ectopic activity of peripheral nociceptors in the pudendal and posterior femoral cut aeneous nerves with repetitive exposure, which resets and desensitizes the Nav1.7 channels involved in the aberrant firing of peripheral nociceptors.
- Increase blood flow to the peripheral nerves by releasing connective tissue and fascial restrictions with hydro-dissection.
- Create space, increase blood flow, and release constricting hypertonic muscular spasms to create a better environment for the pelvic nerves to then heal themselves.
Decreasing myofascial spasm and neurogenic inflammation will ultimately reverse peripheral sensitization and subsequently decrease central sensitization as central pain processing is maintained by afferent nociceptive input.
Our belief for treating endometriosis
In treating endometriosis patients, we believe it is important to look at the integration of the organ systems, with the peripheral and central nervous system, muscles, and fascia. As there is no “silver bullet” or known cure for endometriosis, a multimodal, interdisciplinary medicosurgical approach to a complex multi-faceted disease process may help endometriosis patients not only decrease pain but also improve function. Patient’s endometriosis symptoms can be explained and treated with safe, effective, non-opioid therapies.
A Note to Providers
We encourage gastrointestinal physicians who see women with persistent gastrointestinal symptoms despite a negative work up and appropriate medical treatment to consider endometriosis in their differential. We propose a functional, restorative approach to ameliorate the pelvic pain symptoms associated with endometriosis. Targeting peripheral mechanisms in endometriosis-associated inflammatory pain may lead to improved treatment.
Would You Like to See a Specialist?
Call us at (646) 481-4998 or click to request a regular appointment.