by Dr. Allyson Shrikhande, MD, CMO
WHAT IS CHRONIC PELVIC PAIN SYNDROME?
Chronic Pelvic Pain Syndrome (CPPS) is a condition that affects many individuals, causing continuous or recurring pain in the pelvic region lasting for at least six months. However, its complex nature makes it challenging to pinpoint a single cause or pathology. At PRM, our pelvic pain specialists gather each patient’s story and history of the symptoms they’re experiencing to better determine the cause of their pain.
HOW DOES CHRONIC PELVIC PAIN SYNDROME AFFECT LIFESTYLE?
CPPS is a condition characterized by persistent pain in the pelvic area, which can be debilitating and severely impact a person’s quality of life. It can be caused by multiple factors throughout the body including:
- Gynecologic
- Urologic
- Gastrointestinal
- Musculoskeletal
- Neurological
Abnormal pain signals and tissue responses are believed to play a role in this condition, making it a complex puzzle for both patients and healthcare professionals. However, PRM has been offering an office-based procedure for patients who are showing significant improvement in pain and function.
HOW HAS A RECENT STUDY SHOWN TREATMENT TO BE EFFECTIVE?
As researchers have been looking for ways to reduce the symptoms of chronic pelvic pain syndrome, Alpha-2-Macroglobulin (A2M) has been used in treatments.
A2M is a plasma glycoprotein with intriguing properties, and is known for its ability to inhibit proteases, its antioxidant properties, and its anti-inflammatory effects. These properties have been shown to reduce pain and promote healing in certain musculoskeletal and peripheral neural conditions.
HOW IS THIS TREATMENT LINKED TO INFLAMMATION?
One of the primary contributors to chronic pelvic pain syndrome is neurogenic inflammation, which leads to peripheral and central sensitization. This means that the nerves in the pelvic region become overly sensitive, amplifying pain signals and causing chronic discomfort. Given that A2M targets neuropathic and inflammatory mechanisms, researchers hypothesize that it might hold the key to relieving the pain associated with CPPS.
PELVIC REHABILITATION MEDICINE’S STUDY ON THE TREATMENT FOR CPPS

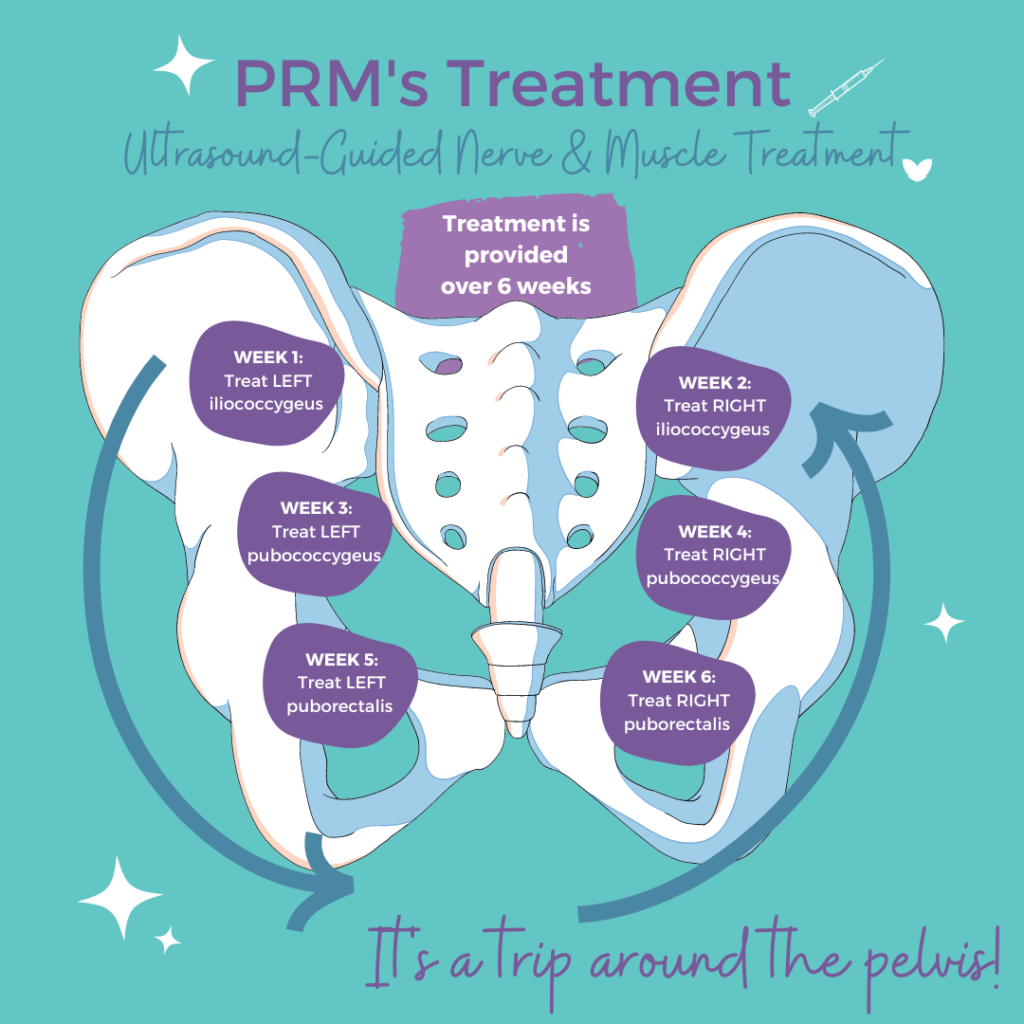
To investigate the efficacy of A2M in treating chronic pelvic pain syndrome, PRM’s team of pelvic pain specialists conducted a study involving 19 patients who were already receiving treatment for the condition. The patients had undergone outpatient ultrasound-guided trigger point injections and peripheral nerve blocks before participating in the study.
Patients who met the study’s inclusion criteria received injections of A2M along with a local anesthetic into a specific area called Alcock’s canal. This area is closely associated with the pudendal nerve, which is believed to play a significant role in CPPS. The injections were performed with the guidance of ultrasound to ensure precision and accuracy.
RESULTS OF THE STUDY
Before and after the A2M injections, the patients’ pain and function were assessed using the Visual Analogue Scale (VAS) and the Functional Pelvic Pain Scale (FPPS). The FPPS evaluates various aspects of daily life, including:
- Bladder and bowel function
- Intercourse
- Walking
- Sleeping
- Working
- Running
- Lifting
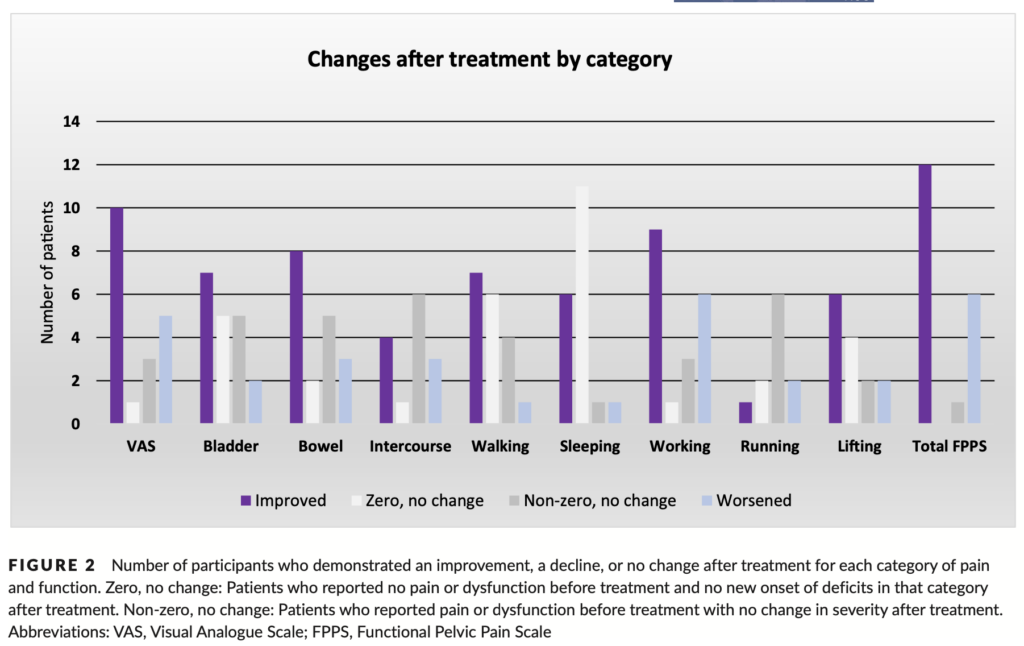
Statistical analyses were conducted to determine the significance of the changes observed after the A2M treatment.
PRM OFFERS RELIEF WITH OFFICE-BASED PROCEDURE AND A MULTI-MODAL APPROACH TO TREATMENT
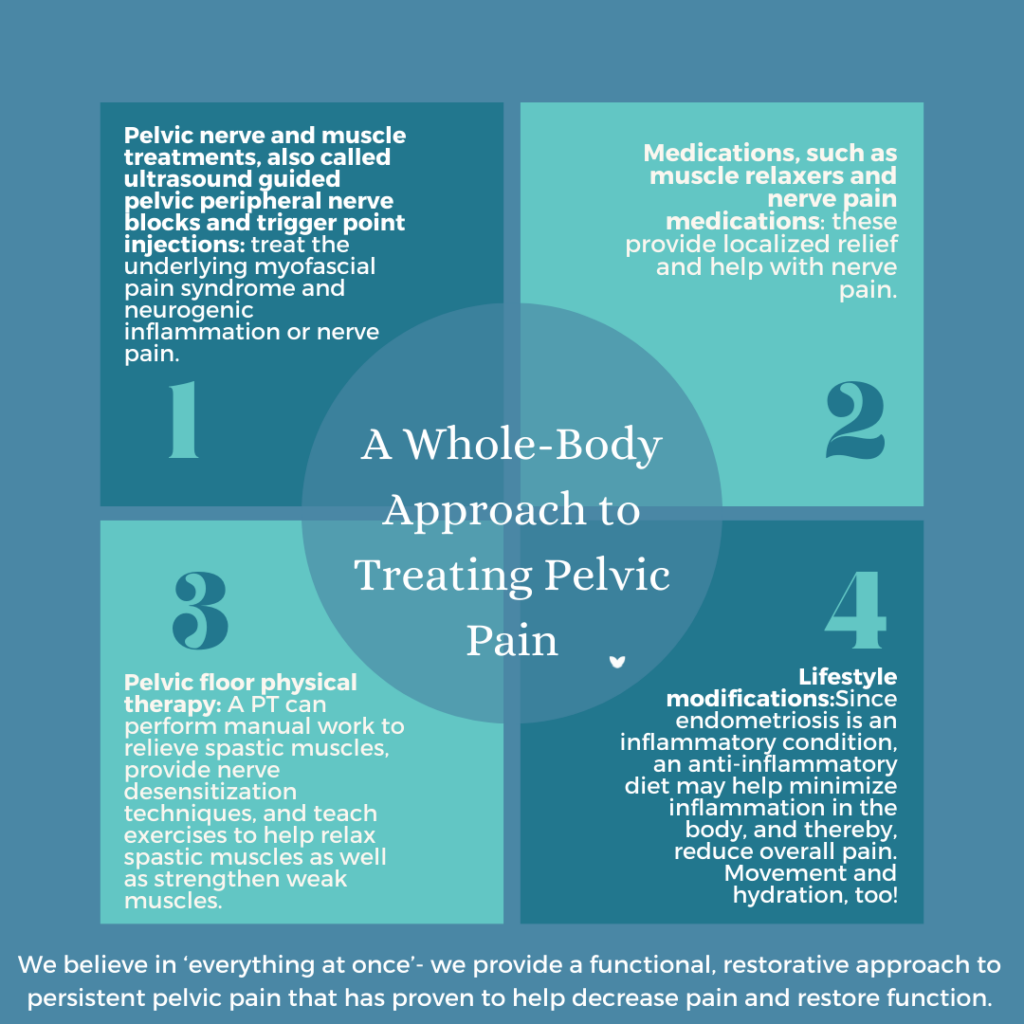
While many people suffer with chronic pelvic pain syndrome, PRM is able to offer an effective, multi-modal approach to treatment which includes this office-based procedure, by targeting the neurogenic inflammation associated with CPPS.
It’s important to note that this study is just one step in the journey to finding better treatments for chronic pelvic pain syndrome. More research and larger clinical trials are needed to confirm the results and understand the full potential of A2M in managing this complex condition. Nevertheless, the findings represent a promising avenue for the future of CPPS treatment, bringing hope to those seeking relief from the burden of chronic pelvic pain.
AUTHOR CONTRIBUTIONS
Brocha Brooks was responsible for data collection, data analysis, and writing of the manuscript. Kim Leishera, Rebecca Aronson, and Melanie Howell contributed to the conduction of study and data collection. Allen Khakshooy was responsible for data analysis and writing of the manuscript. Michael Pico contributed to the writing of the manuscript. Allyson Shrikhande was responsible for the study design, planning, data collection and writing of the manuscript. All authors approved of the final version of the manuscript.
Would You Like to See a Specialist?
Call us at (646) 481-4998 or click to request a regular appointment.