By Dr. Allyson Shrikhande, MD, CMO
Endometriosis is a chronic, systemic inflammatory disease in which tissues that resemble the lining of the uterus begin to grow outside of the uterus. One in ten women is affected. On average, endometriosis takes seven to twelve years to be diagnosed. Treatment options are often scant, and many women undergo unnecessary medical procedures that can be harmful, expensive, and ineffective. At the low end of severity, the disease can be a mild nuisance. At the high end, the impact on a patient’s health can be severe and greatly suppresses their quality of life.
THE INFLAMMATORY CASCADE OF ENDOMETRIOSIS
Endometriosis falls into the category of an inflammatory disease process. Endometrial plaques release a form of “inflammatory soup” into the pelvis which contributes to inflammation around the pelvic nerves. Nerve inflammation is a major contributor to the symptoms of endometriosis including lower abdominal and pelvic pain, pain with intercourse, bladder pain, pain with bowel movements, and more. In addition to causing nerve inflammation and pelvic pain symptoms, this “inflammatory soup” also stimulates the proliferation and growth of more endometriosis lesions.
To put it simply, endometriosis creates inflammation that creates more endometriosis.
Decreasing inflammation in the pelvis is essential to slowing the creation of new endometriosis cells, lessening pain, and improving patients’ function and quality of life. Lowering inflammation also allows the system to return to homeostasis and begin to heal itself.
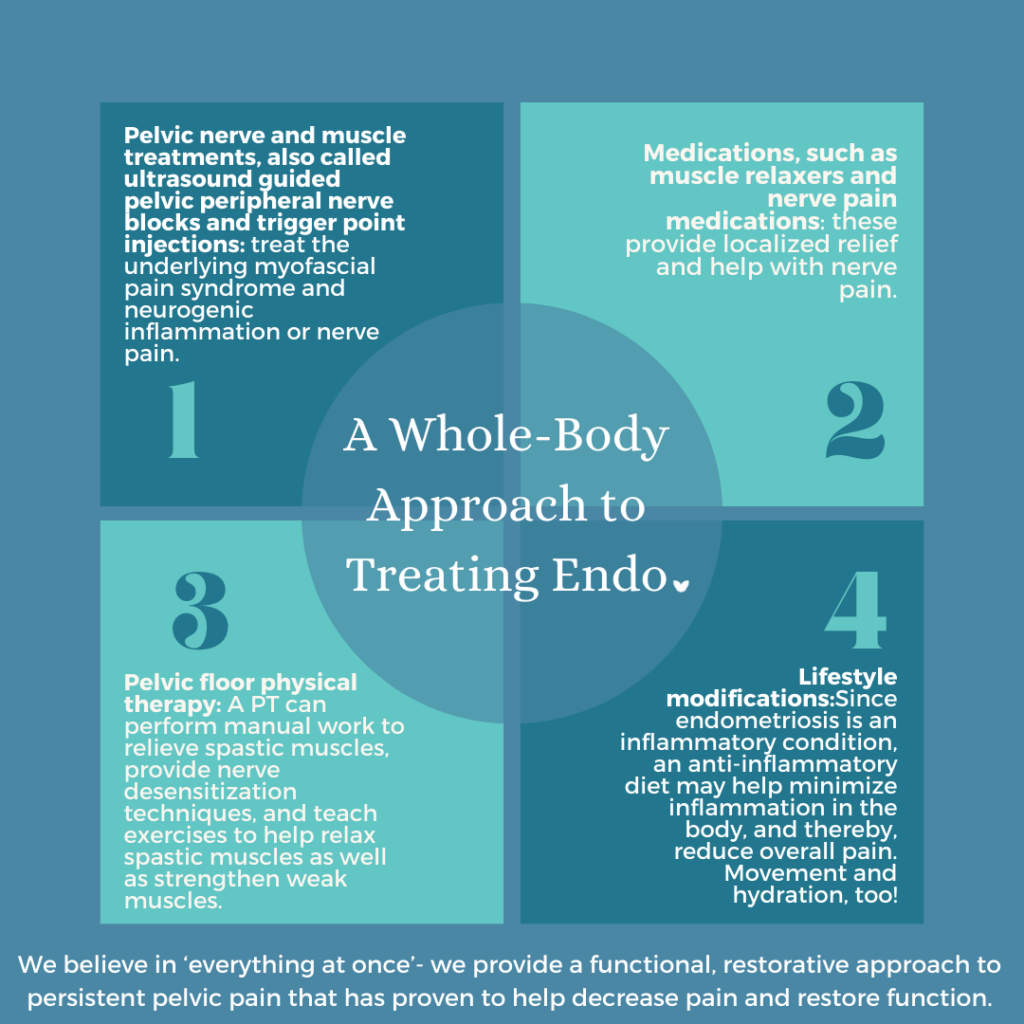
A MULTI-MODAL APPROACH TO HEALING ENDOMETRIOSIS
As the Chief Medical Officer of Pelvic Rehabilitation Medicine, a physician practice that offers a functional and restorative approach to persistent pelvic pain, I am deeply invested in educating women about the broad range of treatment options available for endometriosis. This includes non-operative strategies and ones that avoid opioids or hormones. At PRM, we utilize a unique in-office procedure targeted at decreasing inflammation in the pelvis to promote a healing environment. As endometriosis is a systemic inflammatory process, we also apply a researched whole-body approach by addressing nutrition as well as the mind-body and brain-gut connections.
In-office Procedures to Decrease Inflammation in the Pelvis
Our one-of-a-kind in-office procedure treats both pelvic nerve inflammation and pelvic floor muscle spasms, an often-ignored neuromuscular dysfunction that co-exists alongside endometriosis and other gynecological conditions. This protocol uses ultrasound-guided trigger point therapy to increase oxygen-rich blood flow to the pelvic tissues and nerves. This helps reverse pelvic neurogenic inflammation and allows nerves and tissues to heal. The procedure also softens tight pelvic muscles, releasing pressure and restriction on the nerves.
Additionally, we calm and desensitize “hyperactive” pelvic nerves, which are inappropriately firing and contributing to nerve pain symptoms. Once these nerves can again operate at an optimal level, pain decreases and overall pelvic function improves.
Integrative Nutrition to Reduce Inflammation
Toxicity in the body, accumulated through lifestyle and environmental factors, also causes and maintains an inflammatory state. As endometriosis patients often experience gut dysfunction, it is imperative to include integrative nutrition in our strategy. We help clients detox their overburdened systems, discover the root causes of various physical imbalances, and shift towards a sustainable anti-inflammatory diet.
The diet promotes greens that naturally decrease excess estrogen in the body, as endometriosis is an estrogen-dependent disease process. Estrogen receptors located in endometriosis lesions contribute to the creation of local estrogen, which produces more lesions. As scientists continue to research the exact mechanisms of the disease, our patients can reduce inflammation and regulate hormones through simple, effective lifestyle choices.
A Mind-Body Connection
We understand that our clients succeed best when they’re physically, mentally, and emotionally aligned with their own healing goals. To this end, we emphasize various modalities—individual or group, in-office and online—that help patients reduce stress and inflammatory cortisol levels, connect with other pelvic pain survivors, boost confidence, and retrain their physical reaction to pelvic pain. This ranges from mindfulness-based cognitive therapy to meditation to surgery support groups and intimacy workshops, to name a few.
Endometriosis is a complicated disease that will require more research to fully comprehend and eradicate. But in the meantime, through researched comprehensive strategies, we can empower our endometriosis patients to live a full, happy, and pain-free lives.

Would You Like to See a Specialist?
Call us at (646) 481-4998 or click to request a regular appointment.