A hysterectomy is the partial or total surgical removal of the uterus. This can also include the removal of the cervix, ovaries, Fallopian tubes, and other surrounding structures. It’s a common procedure for women experiencing uterine fibroids, endometriosis, and cervical or ovarian cancer. Hysterectomies are the second most frequently performed procedure for women of reproductive age in the United States. Over 600,000 hysterectomies are performed every year.
While most hysterectomies are straightforward, hysterectomy recovery can be full of surprises. Here are four surprising things that women may not expect after a hysterectomy.
1- Emotional recovery
Women can be left feeling emotionally vulnerable after a hysterectomy. They can experience feelings of sadness, loss, and grief for their loss of fertility. If a woman’s hope of conceiving has been terminated by a hysterectomy, the aftermath can be even more devastating. Often, a woman’s notion of what it means to be a woman—as a mother and desirable partner—is attached to her physiology. A hysterectomy can feel like a loss of feminine identity. It can also feel like a failure, forced menopause, or a sign of premature aging, to name just a few emotions that may resonate after surgery.
Additionally, hormonal changes after a hysterectomy can contribute to mood swings, irritability, sleeplessness, and depression. If a woman’s ovaries are removed at the same time as the uterus, the immediate onset of menopause can cause even more distinct emotional symptoms. Hormone replacement therapy, nutritional counseling, or other types of supplements and medications can ease these emotional fluctuations.
Women experience a spectrum of feelings after a hysterectomy, which should be normalized. Leaning on loved ones and other women, organized support groups, or quality therapy can go a long way in helping a woman recover emotionally from hysterectomy surgery.
Remember, it is essential for patients to seek the support they need if they are struggling. If emotional disturbances are severe, they should immediately contact their doctor.

2- Sexual recovery
Some women are surprised to find their sex lives disrupted by a hysterectomy. Estrogen is a hormone that helps maintain vaginal health and sexual function and is produced by the uterus and ovaries. When the uterus and ovaries are surgically removed, the sudden drop in estrogen can bring about challenging sexual consequences. Potential side effects such as vaginal dryness, painful intercourse, difficulty orgasming, diminished sensation, and a lower libido can add additional stress to a patient in recovery.
But there are definite solutions. A good-quality vaginal lubricant can boost vaginal moisture and elasticity. Estrogen creams can assist with the hormonal changes that bring about lowered sex drive and decreased sensation. And physical therapy can help a patient regain pelvic muscle tone and strength, which can alleviate pain during intercourse or difficulty achieving orgasm.
3- Bowel and bladder function
After surgery, individuals may experience changes in bowel and bladder function such as difficulty urinating, constipation, and incontinence. These embarrassing symptoms can aggravate a woman’s emotional recovery. Pelvic floor physical therapy can diminish pain and retrain muscles in the pelvis to regain control over these basic functions.
4- Lingering pain after hysterectomy
Women with chronic pelvic pain sometimes opt for a hysterectomy. They can be dismayed to discover that the pain is not gone. In fact, between 25-40% of women report continued pelvic pain after hysterectomy.
Consulting with a pelvic health specialist like Pelvic Rehabilitation Medicine can help ensure that surgery is indeed necessary. And if it is, then they can help alleviate postoperative pelvic pain and optimize healing.
What is the recovery time for a hysterectomy?
Hysterectomy recovery time varies depending on the type of procedure and the individual’s overall health.
- For a vaginal hysterectomy, patients can return to normal activities within 2-4 weeks and can return to work within 4-6 weeks.
- For a laparoscopic hysterectomy, patients can also return to normal activities within 2-4 weeks and can return to work within 4-6 weeks.
- For an abdominal hysterectomy, the recovery time is longer. Patients can return to normal activities within 4-6 weeks and can return to work within 6-8 weeks.
A hysterectomy is major surgery. Even after the recommended hysterectomy recovery time, a woman may still experience discomfort, pain, or fatigue. She should resume activities slowly and thoughtfully. Keep in mind that it’s always important to follow the recommendations provided by the surgeon and medical team.
How can a patient alleviate symptoms after a hysterectomy?
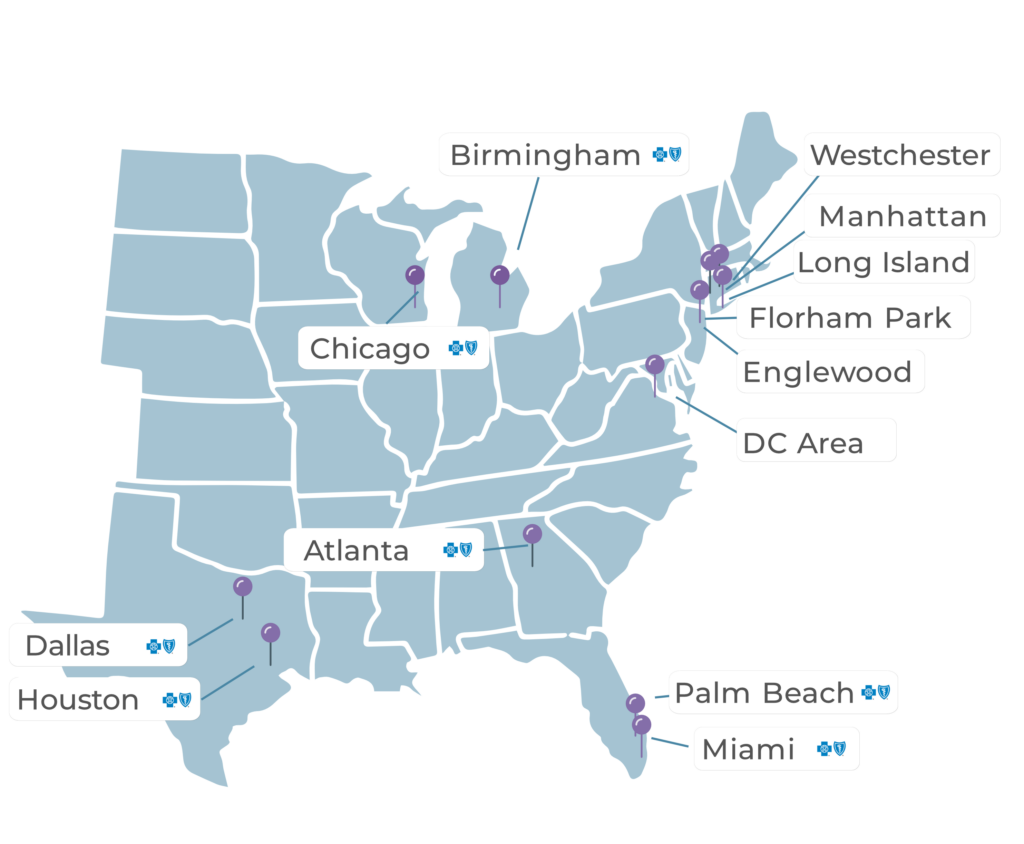
Pelvic Rehabilitation Medicine (PRM) can help with a variety of post-op problems. PRM is a physician practice with offices nationwide that offers a functional and restorative approach to persistent pelvic pain. We have experience treating the repercussions of hysterectomies, both partial and full.
Whenever possible, we use non-pharmacologic and noninvasive interventions that expose patients to less risk than invasive measures or drug therapies. One of the most important of these treatment options is pelvic floor physical therapy.
A multi-modal approach can reduce hysterectomy recovery time
If a patient is experiencing lingering physiological symptoms after a hysterectomy, our team of pelvic pain specialists can help them recover sooner.
Many of our patients come to us 6 months to several years after a hysterectomy and are still experiencing pain. We recommend that if a woman is still enduring extreme discomfort after the three-month mark, she ought to see a specialist. It is simpler to correct certain pelvic issues before they become deeply established in the body.
At PRM, we use a multimodal approach to healing persistent pelvic pain. This can include our pelvic nerve and muscle treatments, managed pelvic floor physical therapy, lifestyle modifications, and medications such as muscle relaxers.
Our unique approach is the first and only of it’s kind in the country and focuses on reversing the inflammation in the pelvic floor, resetting the nerves and muscles, and retraining the pelvic floor.
While hysterectomy recovery can be surprising and sometimes difficult to manage, women do not need to suffer. Please reach out – we can help reduce your symptoms faster and help you regain an optimal quality of life.
Would You Like to See a Specialist?
Call us at (646) 481-4998 or click to request a regular appointment.