By Dr. Allyson Shrikhande, MD, CMO
What is chronic pelvic pain?
Chronic pelvic pain is a complex, multi-faceted condition involving ongoing pain in the pelvic region which affects both men and women. Pain experienced can vary from person to person, ranging in severity (mild or severe), type (dull or sharp), and longevity (constant or intermittent).
How does chronic pelvic pain affect lifestyle?
While many people suffer with chronic pelvic pain syndrome, PRM is able to offer an effective, multi-modal approach to treatment which includes this office-based procedure, by targeting the neurogenic inflammation associated with CPPS.
It’s important to note that this study is just one step in the journey to finding better treatments for chronic pelvic pain syndrome. More research and larger clinical trials are needed to confirm the results and understand the full potential of A2M in managing this complex condition. Nevertheless, the findings represent a promising avenue for the future of CPPS treatment, bringing hope to those seeking relief from the burden of chronic pelvic pain.
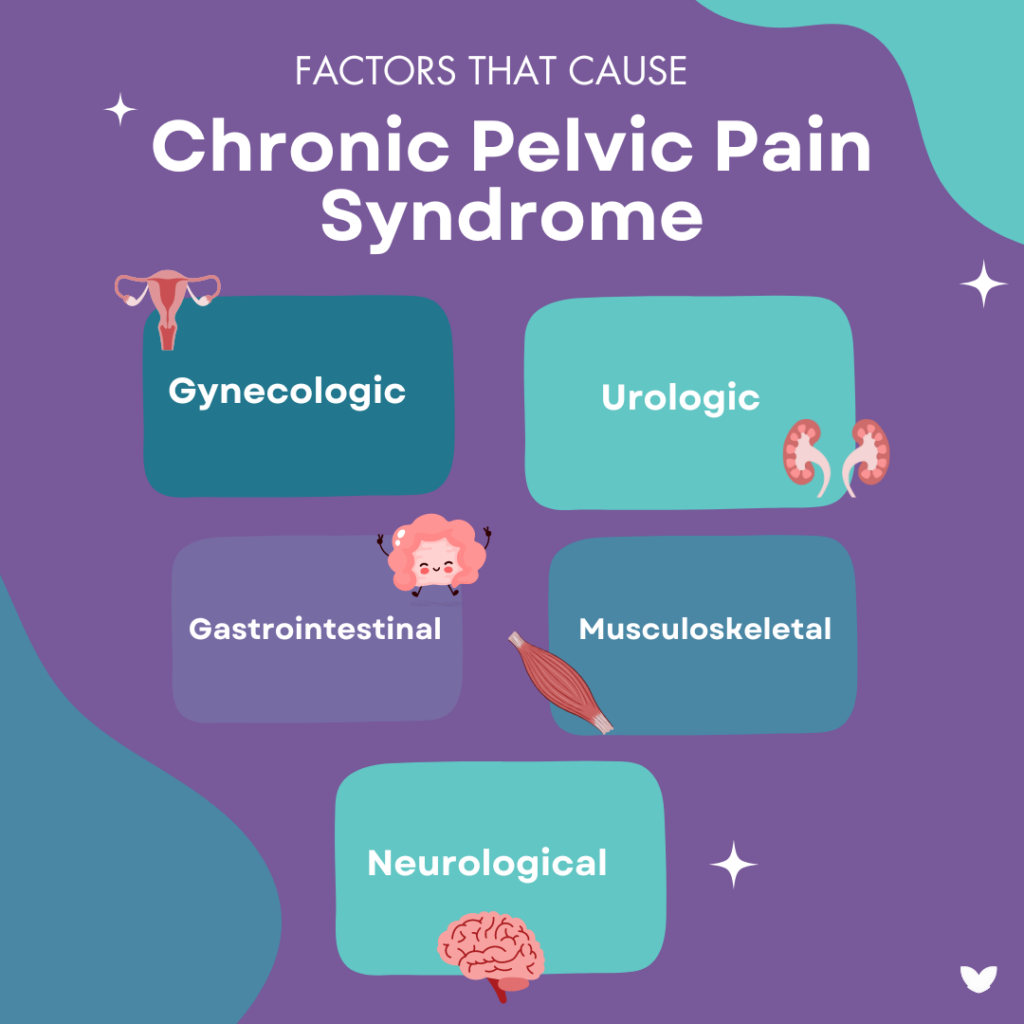
Chronic pelvic pain can seriously affect the lives of both men and women, as it can be caused by gynecologic, urologic, gastrointestinal, and musculoskeletal conditions. This can affect one’s ability to rest, have intercourse, go to work, and any other daily life activities. CPPS also carries a heavy burden on the finances of patients who seek out and receive treatment.
How great is the cost burden associated with chronic pelvic pain?
A study which included research by Pelvic Rehabilitation Medicine determined that the cost for those who seek and receive treatments for chronic pelvic pain is well into the tens of thousands of dollars.
Of 607 patients whose data was used from this study, it was found that the overall cost burden per patient was:
- Surgeries: $15,750
- Diagnostics: $5,264.22
- Treatments: $8,937
On average in this study, chronic pelvic pain diagnosis and treatment costs $29,951 per patient.
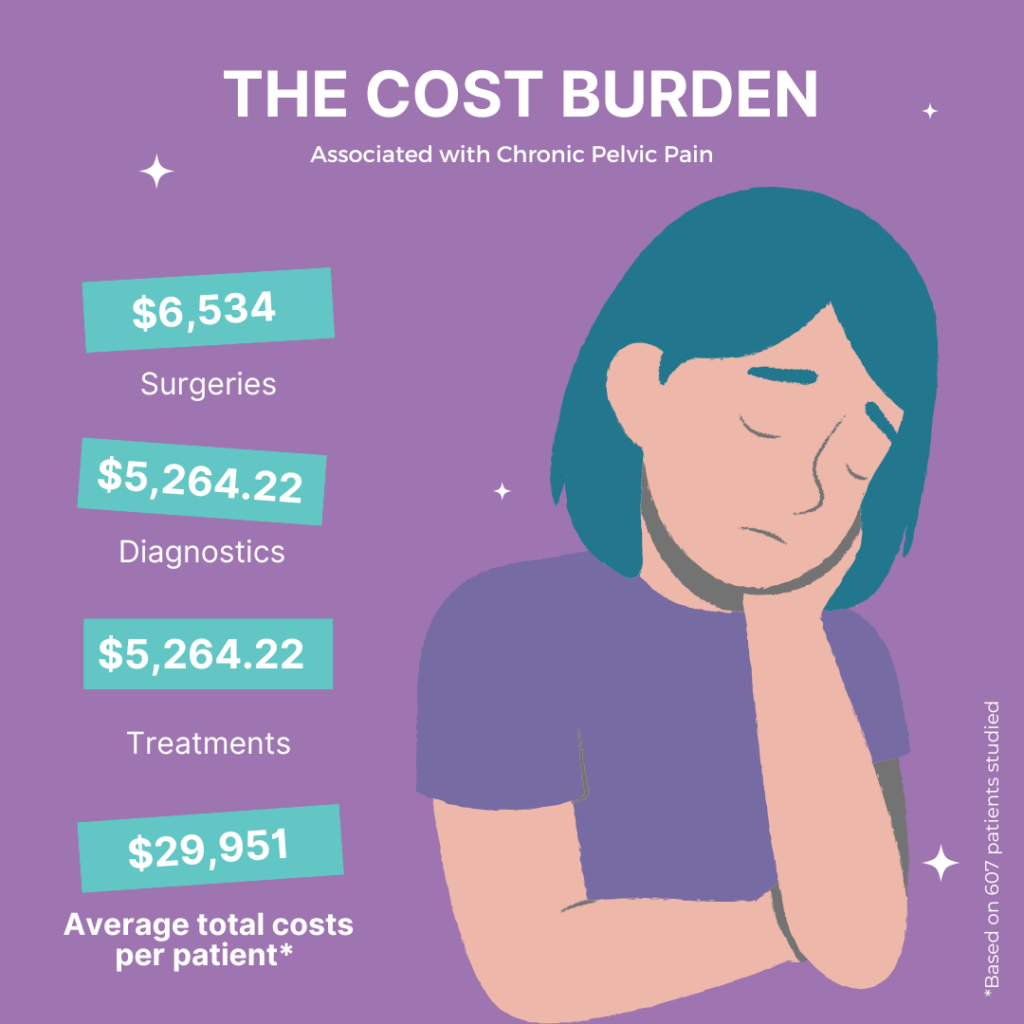
A 2021 systematic review of women with chronic pelvic pain calculated the direct yearly cost per woman to be between $16,970 to $20,898, this includes healthcare, prescription, and indirect costs (lost wages and reduced productivity). For men with chronic pelvic pain, a Northwestern University outpatient urology clinic calculated annual direct costs (via Medicare rates and non-Medicare reimbursements) and lost wages due to absenteeism. Using non-Medicare rates, direct costs were $6,534 per person.
Average indirect costs through lost wages totaled $3,248 per person; the modest value reflects the exclusion of productivity loss while at work.
Who experiences chronic pelvic pain?
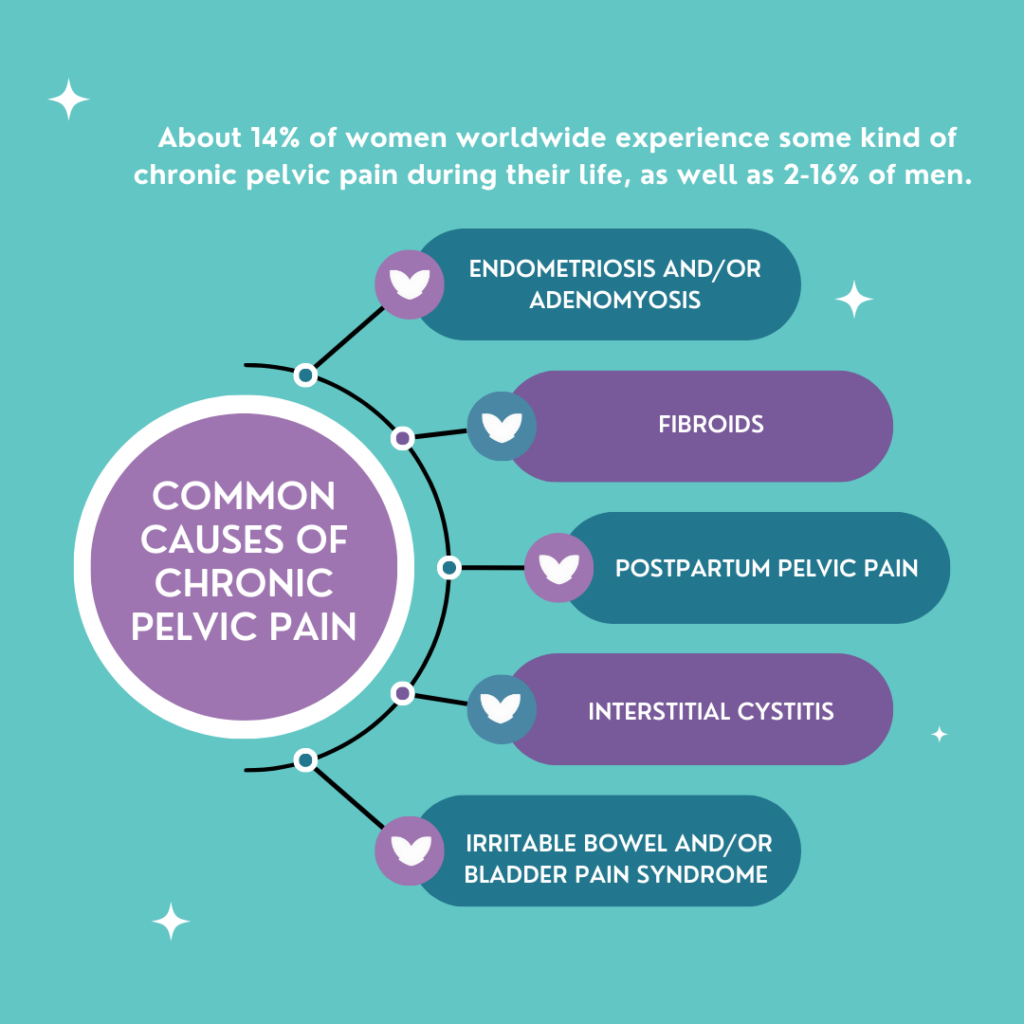
Both men and women can experience chronic pelvic pain, with 14% of women worldwide experience some kind of chronic pelvic pain during their life, as well as 2-16% of men. The most common causes of pelvic pain include:
- Endometriosis
- Adenomyosis
- Fibroids
- Postpartum pelvic pain
- IC
- Bladder pain syndrome
- Irritable bowel syndrome
- Anxiety and depression
If you’re experiencing any of these symptoms, speak to one of our pelvic pain specialists by
scheduling an in-person appointment or free 15-minute phone consultation.
Which conditions causing chronic pain are the most expensive?
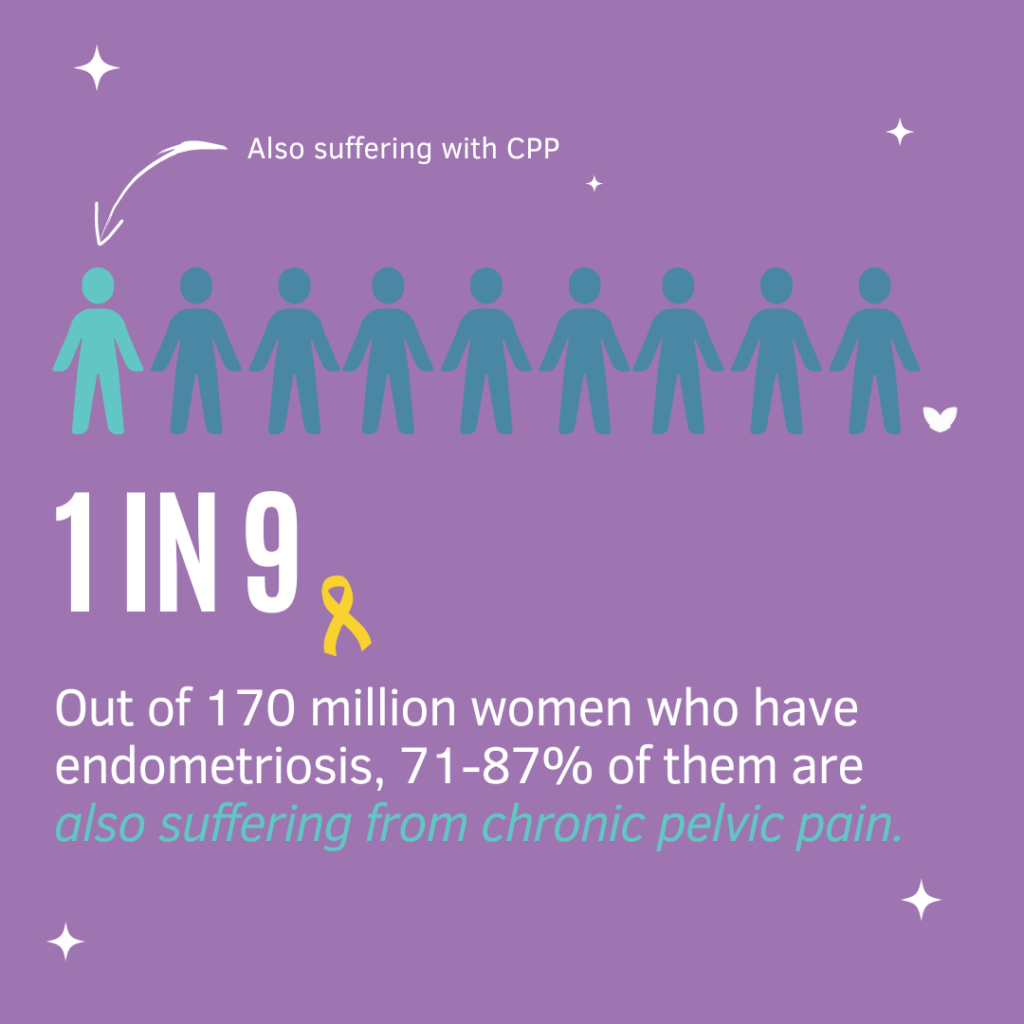
Most of the cost burden data in chronic pelvic pain involves endometriosis, a chronic systemic inflammatory condition typified by lesions of endometrial-like cells outside of the uterus. Endometriosis globally affects 1 in 9 women, and of the 170 million women who have endometriosis, 71-87% of them are also suffering from chronic pelvic pain.
What is the cost burden associated with endometriosis?
In 2018, an evaluation of the cost burden of endometriosis included managing pain symptoms via pharmacological agents and surgical interventions and wages lost from absenteeism. Their calculations demonstrated overall healthcare costs per patient per year as $16,573.
A study found that endometriosis generated a cost burden of $22 billion in the US in the year 2002 (78.6%: direct, 21.4%: indirect). However, in 2010, the economic burden was estimated to be $69.4 billion by analyzing 12 tertiary centers in 10 European Countries (32%: direct and 66%: indirect).

This multi-center analysis did not take into consideration the additional costs on the healthcare system of physical therapy, behavioral therapy, Emergency Room visits, or outpatient treatment procedures. Prolonged symptoms and delayed treatment and diagnosis were associated with higher healthcare utilization.
How does endometriosis affect lifestyle?
A study analyzing 5,879 women diagnosed with endometriosis discovered a positive correlation between symptom severity and hours of employment productivity lost. Women with mild severity reported a weekly loss of 1.9 hours compared to 15.8 hours lost for severe symptoms.
Women also suffer from worsening of quality of life with chronic pain, especially combined with endometriosis, due to difficulties related to pregnancy and obstetric outcomes. Endometriosis patients have significantly higher risks of preterm birth, miscarriage, placenta previa, small for gestational age, and cesarean delivery than women without the disease. 
Do you feel as if you may be experiencing the symptoms of endometriosis?
Take PRM’s quiz to learn more about the disease and it’s affects on the body.
What is the psychosocial impact of chronic pelvic pain?
There is a strong psychosocial impact as chronic pelvic pain patients are affected by anxiety and depression at strikingly higher rates than the general population. A study analyzing 57 articles found women with chronic pelvic pain to be twice as likely to have depression (18.9% versus the control of 9.3%). Another study demonstrated anxiety to be more than four times as likely in CPP patients (29.7% versus 7%).

Depression and anxiety negatively affect the prognosis of chronic pelvic pain and determine the onset of symptoms as they can contribute to central sensitization and “priming of the nervous system”. Mental health diagnoses have been shown to decrease work productivity through absenteeism and presenteeism. The associated costs of depression and anxiety across 36 large countries is calculated to be $925 billion due to the estimated time of 50 million days of work lost due to the onset of depression and anxiety.
How do those suffering with chronic pelvic pain accrue these costs?
Chronic pelvic pain patients can accrue heavy costs by obtaining insufficient relief of their symptoms and consulting many doctors without receiving a precise diagnosis or appropriate management for many years.

Unfortunately, many patients can have the impression of being abandoned by the medical profession. Currently, the treatment of chronic pelvic pain and its related comorbidities is a multimodal interdisciplinary comprehensive outpatient protocol involving:
- Pharmacological agents
- Physical therapy
- Behavioral health
- Lifestyle modifications of diet, exercise, and sleep
- Ultrasound guided peripheral nerve blocks, trigger point injections
- Surgical interventions, if conservative management fails to resolve symptoms
How can we alleviate the cost burden for chronic pelvic pain sufferers?
Chronic pelvic pain was found to have a large cost burden for in-net- work services which includes treatments, diagnostics, and surgeries.
These in-network services are often redundant and unnecessary. This leads to an increase in healthcare costs for CPP patients while simultaneously negatively affecting their quality of life and functional capacity. This publication highlights the societal and individual cost burden of CPP in order to encourage physicians to understand CPP and its multifaceted complex nature so that patients can be treated with better outcomes and minimize the costs associated with systematic healthcare utilization from delayed diagnosis and treatment.
A streamlined interdisciplinary multimodal approach to a more rapid diagnosis and treatment of CPP patients with a clearly delineated treatment algorithm will improve the quality of life of CPP patients and decrease the current dis-utilization of the healthcare system.
More About the Chronic Pelvic Pain Cost Burden Study
Our analysis sets the stage for future investigations involving data on costs of medications that patients have tried prior to presenting to us and costs associated with work hours lost.
See our comprehensive study here: https://pubmed.ncbi.nlm.nih.gov/36757947/
Would You Like to See a Specialist?
Call us at (646) 481-4998 or click to request a regular appointment.