by YOGITA TAILOR, DO
I have gotten often asked what is the best treatment for chronic pelvic pain syndrome or chronic pelvic pain? I would say that is like a trick SAT question where there is more than one answer!
The pelvis – which includes the area in between the belly button and the upper thighs — has a lot of parts to consider. We have our organs like our bowel, or bladder, as well as uterus and prostate respectively for women and men, but then there is also a full network of muscles which support our organs, as well as our core and our bowel/bladder function, and a very complex network of nerves.
When we are treating chronic pelvic pain, we want to keep all of this in mind!
WHO TREATS CHRONIC PELVIC PAIN?
First and foremost, I would say you need to have your collaborative medical team. This can include your primary care, physician, gynecologist, urologist to help check for any underlying medical issues. Other important members of the team should also include a pelvic health specialized therapist, and if possible, a physiatrist, like me, who specializes in chronic pelvic pain.
The role of this team is not only to help figuring out if there is a specific cause(s) for the pain, but also assess how this pain affects your function. This can include things like working, sleeping, exercise, bowel and bladder function, pain, or difficulty with intercourse, as well as how all of this impacts our mood and social life. Often, more than one facet of our life is affected when we are dealing with chronic pelvic pain.
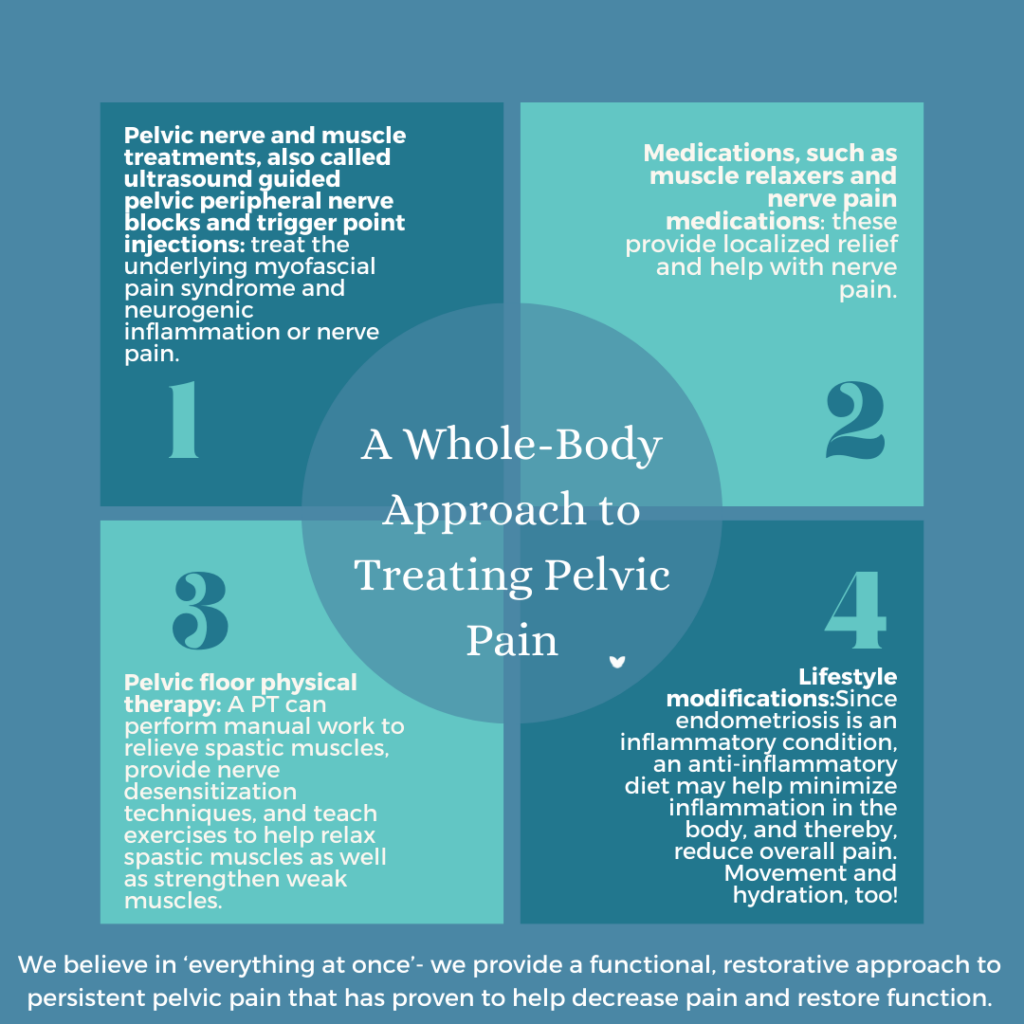
To help treat this, we need to address a few different things simultaneously for the most impactful, efficient, and long-lasting relief.
- Breathing patterns. Diaphragmatic, breathing, also known as deep belly breathing can be a wonderful and easy way to help relax the pelvic floor as well as calm down the nervous system.
- Posture. Our pelvic floor with our abdominal and back muscles, make up the core and so proper posture and engagement is very important when we are trying to break patterns the pelvic floor.
- Internal muscles. While mini exercises and stretches can help our external muscles. Sometimes our internal muscles known primarily as our levator ani muscles can be a little bit more difficult to reach a pelvic health therapist can help can assess these muscles through manual therapy to help lengthen and relax these muscles to calm down the chronic attention.
- Nutrition. There are many foods that can promote inflammation, as well as constipation. This can cause or amplify chronic pelvic pain. Sometimes having a nutritionist on board to help guide a gut-healthy diet can be so impactful.
- Mood and stress. From work to family stress to traffic to pain, there are so many factors in our day that can rev up our whole nervous system. Better control of our stress and anxiety has been shown to help calm chronic pelvic pain. Sometimes having a behavior specialist to help guide. This can also be very beneficial.
- Medication. For some, medications may need to be part of the treatment plan, often, just for temporary to help calm down the nerves, the muscles, the inflammation, the hormones. This decision can be made by you and your physician.
- Injections. When pain has been present for a long period of time more interventions are sometimes needed. This can include a series of external ultrasound, guided nerve blocks and trigger point injections, such as the ones we do in our office.
- Surgery. While in the ideal situation we want to avoid surgery, sometimes this may be inevitable depending on the root cause and other factors. Again, this is something to discuss in depth with your physician to determine if this is the right step for you.
At PRM, we always remind patients: pain is never normal. If your pain has been normalized or you are not being heard by your provider, you should know that you have options. Give us a call and let us help!
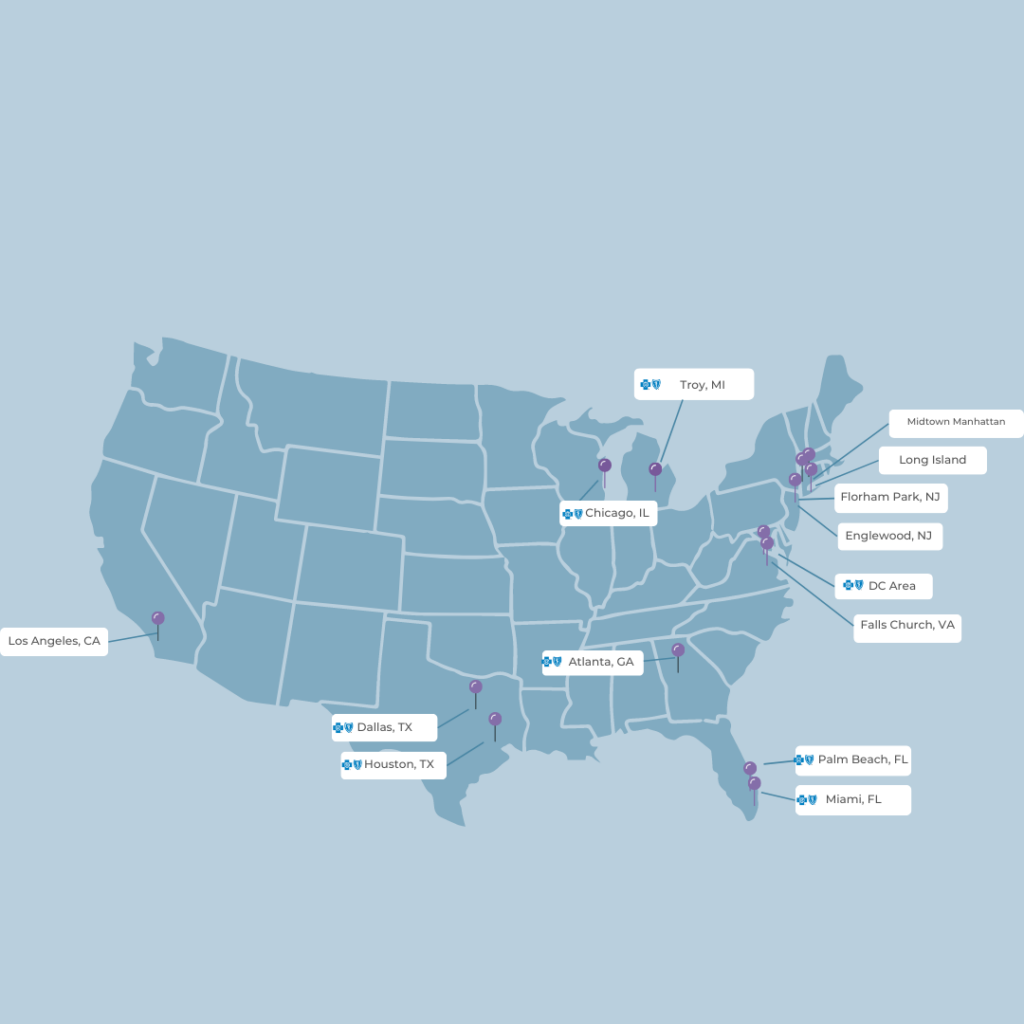

Would You Like to See a Specialist?
Call us at (646) 481-4998 or click to request a regular appointment.